Six years ago, the airwaves were alive with Lipitor ads. Lipitor, a statin and the largest selling drug in the world at that time, was being challenged by other less expensive statins that had gone off patent, so Pfizer, the manufacturer, was blanketing the media in an effort to keep sales humming.
Pfizer had a series of ads featuring Dr. Robert Jarvik, one of the developers of the first artificial heart. These ads were a first in that a real doctor had never appeared in an ad touting a drug. As I posted at the time, Pfizer and Dr. Jarvik got into some trouble because they all played a little fast and loose with the truth about Dr. Jarvik’s credentials.

Aside from the misrepresentation by both Pfizer and Jarvik, one of the claims many of these ads made was that by taking Lipitor you could reduce your risk of heart disease by 36 percent. Sounds pretty good. I would like to reduce my risk of heart disease by 36 percent as did millions of people who went on the drug.
These ads weren’t technically misleading, but they didn’t tell the whole truth, because the 36 percent reduction in heart attack risk was what’s called a relative risk reduction.
Relative Risk
Relative risk is always stated as a percentage. Let’s say we do a study in which we randomize 200 subjects in two groups of 100. One group (the study group) takes a drug, and the other (the control group) takes a sugar pill. We keep the subjects in the two groups on their pill regimen and wait for, say, ten years to see what happens. After ten years, we find that 90 people in the group taking the sugar pill died while only 60 people taking the drug died.
We can then do the following calculation. 90 − 60 = 30. 30 divided by 90 = 0.33. Converting 0.33 to a percentage = 33 percent. Which is the relative risk. If this were an actual study, you could say people taking the drug reduced their risk of dying by 33 percent.
Would this be important? Absolutely. In this case as least. Why? Because 150 people out of 200 died. This means most of the people in the study died, so a 33 percent reduction in risk is huge. I would be all over this drug in a heartbeat.
So what’s the problem, then, with the 36 percent reduction in risk found in the Lipitor study? And why shouldn’t people be begging to go on Lipitor?
Because they need to know the absolute risk before the relative risk becomes important.
Absolute Risk
The absolute risk is simply the total risk for whatever is being studied. In our made up example above, the study end point we were looking for was death. In that example, 150 out of 200 died. So if you were a subject in that study, your absolute risk of dying would be 150 divided by 200 or 75 percent, which is very high.
If your absolute risk of crashing during a commercial airline flight were 75 percent, you would never fly. But if you absolutely had to fly, and one airline offered a 33 percent reduction in risk of crashing (relative risk), you would be stupid not to fly that airline.
To make sense out of relative risk, you’ve got to know the absolute risk.
Let’s go back to our Lipitor claim.
The 36 percent relative risk reduction figure came from a study published in Drugs titled Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial–Lipid Lowering Arm (ASCOT-LLA): a multicentre randomised controlled trial.
This study was a subset of a larger study in which about 20,000 subjects with high blood pressure and three other cardiovascular risk factors were randomized into two groups, the subjects in each of which got one of two blood pressure lowering medications. From this larger group, a little over 10,000 subjects were found who had cholesterol levels at or below 250 mg/dl (6.5 mmol/l). In addition to the blood pressure medications, half of this group got 10 mg of Lipitor (atorvastatin) per day while the other half got a placebo along with their blood pressure medication.
In the Lipitor/placebo arm of this study, the endpoint was defined as a non-fatal heart attack or death from heart disease.
After about 3.3 years, this arm of the study was discontinued because there were a significant number of either heart attacks of deaths from heart disease in the placebo group, and the researchers felt it was unethical to continue the study.
When the data were examined, it turned out that the group taking Lipitor experienced a 36 percent decrease in relative risk for heart disease. Thus the barrage of ads for Lipitor that followed.
Even websites aimed at doctors, using info from the Lipitor package insert, showed graphics designed to make any doctor grab for the Lipitor pre-printed prescription pad. This graph is 100 percent accurate, but, as we shall see, hugely misleading.

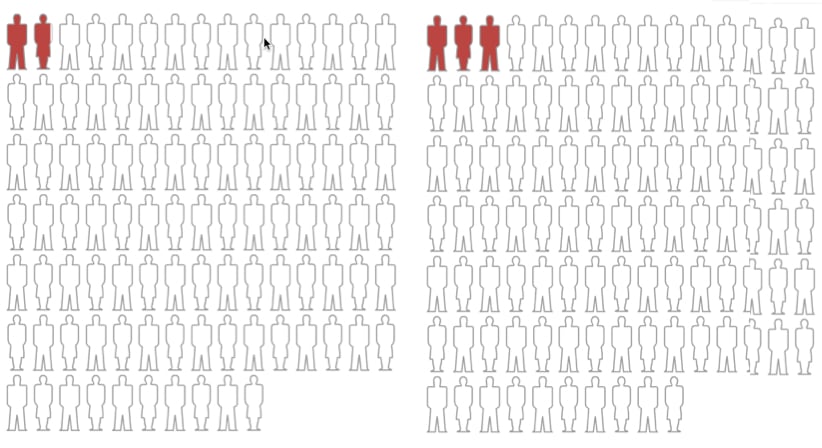
Figure 1 below is a graphic showing what that 36 percent relative risk looks like.
Figure 1. Relative risk of 36 percent with a large absolute risk.
Pretty impressive, isn’t it? Makes you wonder why anyone wouldn’t want to take Lipitor. Problem is, Figure 1, which I made up, shows a relative risk differential of 36 percent, but it also shows a large absolute risk.
Looking at Figure 2 below, which shows the actual absolute risk of experiencing a heart attack or dying from heart disease in this study, you can see that the 36 percent relative risk reduction is accurate. But does it really make you want to stampede to the pharmacy to pick up your Lipitor? Remember, these subjects all had high blood pressure and two other risk factors for heart disease, yet their absolute risk is pretty low. Would you want to take a medicine that could give you muscle aches and pains along with muscle wasting, short term memory loss and possibly fatal liver or kidney damage based on the absolute risk shown in Figure 2?
Figure 2. Relative risk of 36 percent with actual absolute risk in the Lipitor study.
If you compare Figure 1 to Figure 2 above, both of which have the same relative risk, you can readily see that the absolute risk is extremely important. If the absolute risk is high, as it is in Figure 1 at the top, then the relative risk becomes important.
If, as in Figure 2, the real Lipitor vs placebo graphic, the absolute risk is small, then not so much so.
Both Figure 1 and Figure 2 show the same relative risk, but not anywhere close to the same absolute risk. Which is why you always want to know the absolute risk before you make a decision on anything based on relative risk. Because absolute risk is usually pretty low in drug studies, the pharmaceutical industry typically uses the relative risk number to sell their medicines.
In the case of statins, most people go on statins because what they really fear is dropping dead of a heart attack, and they feel the statins are protective.
What happened in this study? There were two more deaths in the placebo group than in the Lipitor group, but that number wasn’t statistically significant. Figure 3 below is a graphic showing the absolute risk of having a fatal heart attack in the Lipitor trial.
Figure 3. Relative and absolute risk of fatal heart attack in the Lipitor study.
Not a huge absolute risk.
Let’s look at another example that is much more dramatic than the Lipitor study above.
I pulled a paper from the New England Journal of Medicine (NEJM) looking at coronary artery calcification (CAC) scores and risk for having a heart attack.
Approximately 20 percent of the plaque in coronary arteries is composed of calcium, which shows up on X-rays. But since the heart is constantly in motion, it’s difficult to see the calcium in standard X-rays of the chest. Specialized CT machines, however, can take extremely fast photos of the heart and actually see the calcium in the coronary arteries. A computer program then converts this calcium into a score, which is simply a number. If you have a zero score, you have no calcium accumulation, which means you probably don’t have any plaque to speak of. You could have some soft plaque that hasn’t yet calcified, but a zero CAC score is definitely a good one.
The NEJM study looked at CAC scores of 6,722 subjects and broke them out into one of four groups. Zero, CAC score of 1-100, CAC score of 101-300, and CAC score of greater than 300. These groups were followed for about 4 years on average for the main endpoint of the study, which was a major coronary event, defined as a heart attack or death from coronary heart disease.
You can see the relative and absolute risk in the graphics below. Upper left is zero CAC score. Upper right, 1-100 CAC score. The lower left is 101-300 CAC score, and the lower right is greater than a 300 CAC score.
 Figure 4. Relative and absolute risks for various CAC scores. Zero upper left. 1-100 CAC upper right.
Figure 4. Relative and absolute risks for various CAC scores. Zero upper left. 1-100 CAC upper right.
101-300 CAC lower left. Greater than 300 lower right.
As you can see, the risk for a major coronary event is negligible with a CAC score of zero. And the risk increases as the CAC scores go up. The subjects in this study who had CAC scores above 300 experienced 19 times more major coronary events than did those with zero CAC scores. Which would mean a 300+ CAC score carries a relative risk of 1900 percent* as compared to a zero, which is humongous. But looking at the absolute risk tells a different story.
I’ve seen patients with 300+ CAC scores come unglued. Granted, it’s not a score you want to see, but it doesn’t mean you’re going to die the next day. A lot of people feel that way, though. Which is why knowing the absolute risk is important before you decompensate over a high relative risk for this or any condition.
If you would like to play around with these absolute and relative risk graphics, you can do so at this site.
Keep the site bookmarked, so the next time you come across a relative risk, look up the actual risk and graph it. Only then will you know the true risk involved.
_______________________________________________________
*I used a relative risk score based on the raw data from the study. If you look at the actual study (linked above), you see different relative risks than what I have. The ones in the study are lower because the authors extrapolate the data out longer and take into account when the events happened. So, if you happen to have a high CAC score, your risk is lower than what I show above, which was strictly for illustrative purposes.




If only there was a substantial database (WHO?) with both absolute & relative risks. That really could start “evidence-based” medicine!
I would like to be able to make a proper comparison between my risk of ischaemic stroke due to Atrial Fibrillation versus my risk of death from from haemorrhagic stroke or from arterial calcification run rampant because of an AVK anticoagulant reducing/preventing carboxylation of MGP.
I’m not sure I can trust my new cardiologist to do this for me & I certainly could not trust my old cardiologist.
Kevin, that’s probably too intelligent an approach to ask for in this country at this time. Sad but I think it’s true.
Is there a well-informed holistic M.D. in your area?
Mine helped me immensely.
Dr Eades – are there any circumstances under which you would prescribe a statin to a patient?
Also – do you give any weight to high LDL-P and high LDL-C?
The figures you ask about are not diseases. They are lab values.
Off the top of my head, I can’t think of an instance in which I would prescribe a statin. That doesn’t mean that if I were presented with a situation in which there was strong absolute risk and decent relative risk that I wouldn’t prescribe. I just haven’t encountered the situation yet in which the risk reduction would offset the potential harm.
SO – what about a person with FH? What would you do about that?
Perhaps. But would depend upon what kind and whether or not the patient responded to nutritional therapy.
nutritional therapy like?
Bergamot, Berberine, and Amla perhaps?
http://www.nutritionaloutlook.com/article/cholesterol-control-3-13607
Bergamot, maybe. But I meant more of a dietary change rather than supplementation.
That tool is so handy, thank you for breaking this down for us in such an understandable way. Trying to explain to someone who doesn’t enjoy digging into the actual data can be an exercise in frustration, and this clarifies succinctly and visually, as well.
Good article that even my physician friends should read. The lack of critical analysis skills among physicians is lower than many know.
Also I would point out that the graph you provided is a hazard ratio, not relative risk. As you know a Cox Proportional Regression model (hazard ratio) is the most educated wild ass guess we have!! LOL! And thanks for the link, I will use that in the future for sure in explaining such things to friends.
Thanks.
What I provided are relative risks, which are simply the ratio of events occurring in the treatment group vs the control group. Hazard ratios are more difficult calculations. Here is a nice article on the difference (pdf).
Understand and thanks for the reply. The graph I’m seeing on my end shows an HR-0.64. And yes they are more difficult and provide different information, but they are still a very educated guess. I’m only pointing it out because it could be relevant (to some ready this) but doesn’t change the juxt of your piece, which is good in my opinion. Although we don’t always agree I do enjoy your writing and appreciate the information you put forth.
I just can’t believe there is someone out there who doesn’t always agree with me.:)
Me too!!
Thanks again for the link, that’s a fun tool that I will use when appropriate to help illustrate to many who don’t take interest in such.
Dr Eades
Any thoughts/comments on this
http://www.genengnews.com/gen-news-highlights/cholesterol-levels-in-blood-linked-to-amyloid-deposits-in-brain/81249300/
“December 30 in JAMA Neurology, in a paper entitled “Associations between Serum Cholesterol Levels and Cerebral Amyloidosis.” The paper described how the scientists evaluated 74 diverse male and female individuals 70 years and older who were recruited from California stroke clinics, support groups, senior facilities, and the UC Davis Alzheimer’s Disease Center. The study’s participants included three individuals with mild dementia, 33 who were cognitively normal, and 38 who had mild cognitive impairment.
The participants’ amyloid levels were obtained using a tracer that binds with amyloid plaques and imaging their brains using PET scans. Higher fasting levels of LDL and lower levels of HDL both were associated with greater brain amyloid—a first-time finding linking cholesterol fractions in the blood and amyloid deposition in the brain.
Charles DeCarli, director of the Alzheimer’s Disease Center and an author of the study, said it is a wake-up call that, just as people can influence their late-life brain health by limiting vascular brain injury through controlling their blood pressure, the same is true of getting a handle on their serum cholesterol levels.
“If you have an LDL above 100 or an HDL that is less than 40, even if you’re taking a statin drug, you want to make sure that you are getting those numbers into alignment,” DeCarli said. “You have to get the HDL up and the LDL down.”
“Besides raising the possibility that people receiving cholesterol treatment should continue it regardless of their cardiac status, if they are developing memory loss, the study “also suggests a method of lowering amyloid levels in people who are middle aged, when such build-up is just starting,” added Dr. Reed. “If modifying cholesterol levels in the brain early in life turns out to reduce amyloid deposits late in life, we could potentially make a significant difference in reducing the prevalence of Alzheimer’s, a goal of an enormous amount of research and drug development effort.”
Although the researchers did not study the mechanism for how cholesterol promotes amyloid deposits, they did note that such considerations “must account for the fact that essentially all central nervous system cholesterol is locally synthesized and that there is minimal exchange of HDL-C particles and essentially no exchange of LDL-C and very low density lipoprotein cholesterol-C particles across the intact blood-brain barrier.”
Serum cholesterol levels, speculated the authors, may be related to or interact with chemical species that can both efficiently traverse the blood-brain barrier and also influence amyloidosis. Alternatively, “systemic hyperlipidemia may damage the blood-brain barrier via inflammatory and other mechanisms, with consequent leakage of serum cholesterol, inflammatory cytokines, and other amyloidogenic factors.”
The amyloid theory of Alzheimer’s is rapidly becoming passé, so I’m not sure what relevance this has to statin use.
Off topic, but maybe some good news:
http://feinmantheother.com/2013/12/27/american-diabetes-association-embraces-low-carbohydrate-diets/
Actually, the Richard Feinman article is satire. He’s writing as if he were the ADA doing the right thing based on the data. Instead, unfortunately, they are sticking with their old recommendations.
I wonder if the CAC data controlled for the balance among vitamin C, vitamin D, and calcium.
An excess of vitamin C causes calcium to be leached from the bones into the blood, and it is subsequently deposited in soft tissues, notably joints. It occurs to me that blood vessels (and bacterial plaques) may qualify as “soft tissues”.
I doubt it. The article was mainly about assigning risk to various CAC scores, not the mechanism for calcium buildup.
Seems to me if you don’t take the mechanism into account, you don’t know how to approach the buildup. Kinda like buyings nails to fix a building that’s falling down, without taking into account that the building is made of bricks.
can you pls define what is excess vitamin c? also pls post a link to the paper from which you got the info about calcium being leached fm the bones due to excess vitamin C. thanks.
Dr. Eades,
Thanks for explaining this. I work in the marine industry as an operator, and what I do is risk analysis and management as a daily part of my job. Unfortunately the concept of risk is poorly understood by the masses.
You wrote:
Never were truer words written. I can’t tell you how often I get blown up on Twitter or via email whenever a study comes out showing a relative risk of 20 percent for whatever. Scares people to death, and they don’t have a clue as to what it really means.
A simple, yet very clear example of the difference between “absolute” and “relative”…
Would you rather have 100% of *my* money, or 5% of Warren Buffett’s? 🙂
Nice example. Thanks.
I would love to know the difference in relative and absolute risk for stroke after AFib. My husband has had 3 episodes that required hospitalization since July. He has no other heart issues, no blockages, no valve problems, etc. He has nasty side effects from Xarelto and also a host of other drugs they have put him on. He is otherwise healthy and is a runner. He has not been able to run since July because of all the side effects of the drugs. They are turning him into an invalid. I would love some more information on how to approach the subject with his cardiologist. We are open to going to another town to another cardiologist if necessary. I can’t find any site that gives study results on Xarelto. He is also on a beta blocker but he has a normal lower pulse rate being a runner so they could not give him the amount they wanted due to his pulse bottoming out. If anyone on this blog has any information please post! Thanks
Just for grins, I made a quick run through the internet to see what I could find.
This site tells me that 795,000 suffer strokes in the US each year. This site tells me one out of every five strokes happens in a person with Arial fib. The same site tells me there are roughly 2,000,000 people in the US with atrial fib. From these data, I can calculate that of the 2,000,000 people with atrial fib, 159,000 of them will have a stroke in a given year, which calculates to about 8 percent.
Going to the study on Xarelto, I find that the drug reduces strokes to about 1.8 percent per year. Warfarin, the old standby that is no longer on patent, reduces stroke to about 2.2 percent per year.
If you go to the calculation site I mentioned in the post, enter 8 in the numerator and 100 in the denominator and you can see the absolute risk for stroke in someone who has atrial fib. Do the same exercise with 1.8 in the numerator and 100 in the denominator to see the absolute risk with Xarelto. You can do the same with 2.2 and 100 to see the absolute risk with warfarin. Compare the graphics you come up with to see the relative risk.
These calculations are for educational purposes only and not meant to be a substitute for discussing with your physician. You might want to take the graphics and calculations to your doc. Maybe warfarin would be a better choice since there isn’t much of a difference between it and Xarelto. But discuss with your doc before making any changes.
Thank you for the info. We will take it to the cardiologist in 3 weeks and discuss.
Unfortunately, most of the people hearing this type of news or advertising (to different drugs, or other products) are not interested to question what they hear.
They take it for granted. The same concept is often applied in weight loss when relative fat loss is used compared to absolute fat loss.
Nonetheless, I think those who are really interested into knowing something will dig deeper and get closer to the “truth”.
Thanks for bringing this up doc!
Plus, we worry a lot about specific risks, thinking maybe we can reduce them. But for a majority of people, death will come out of left field, not from some “big” risk like heart disease or cancer. That is, we jack our lives around trying to deal with some risks, but we can’t (don’t) do much about the countless small risks that, in the aggregate, are more likely to kill.
Besides to the moderate reduction in absolute risk, I do have another issue with respect to the ASCOTT-LA trial condidered: in the abstract (I’d like to be able to access the whole paper), we are told that the median follow-up was of 3.3 years. This means that for half of the subjects (that’s 9671 patients, by any means a small sample) there’s information available for a longer period… I wonder to what extent the outcomes on this are discussed in the article.
Also, it is questionable to have stopped the trial before time; however good the intentions might have been. It is not possible to know wht the outcome would have been after the 5 years originally proposed. A bit like stopping football matches at half time if the home team is winning, isn’t it?
Stopping the game at halftime when the home team is winning is a terrific analogy to what the authors of this study did. I would have made an issue of that had I been critiquing the study, but I was simply using it to show the difference in relative and absolute risk. I wanted to use that particular study because there had been such medial hype over the 36 percent reduction in relative risk.
Dr. Eades, you forgot to mention that ending the study after 3.3 years, right after enough people in the placebo group had died to show an advantage for the Lipitor group, is highly unscientific. I’m not buying the claim that it would have been “unethical” to continue the study, especially in view of the small number of people who actually died. It clearly introduced a bias to end it then, before someone in the Lipitor group had had a chance to die and even the score.
For a study to achieve scientific status, its duration (and all other experimental parameters) must be established in advance.
Totally highly unscientific. Usually studies are stopped when the mortality or morbidity is so great in the treatment group as compared to controls that it presents an ethical dilemma to keep going. It’s not usual to stop one because the treatment is so successful.
HI Dr. Eades.
Thank you for your website. I think my parents are finally asking questions about statins.
I thought you might be interested in this interview with John McDougell ‘The Starch Solution’
was on ‘Coast to Coast AM’ last week.
What to make of all this. Everybody is SO sure–somebody must be wrong–right??
You must have forgotten the link to the McDougall interview.
@cecilhenry
http://www.coasttocoastam.com/show/2013/12/23
I looked it up and found that you cannot access the actual interview unless you sign up for membership. Doesn’t matter, the write up says enough and I’m sure Dr. Eades already knows about Dr. McDougall, anyway. I’m looking forward to his response.
Here’s the link to the interview with McDougall
Its on youtube easily available.
http://www.youtube.com/watch?v=b-MSy6hcsrQ
Doesn’t Dr Eades disagree quite strongly with the McDougall diet??
Yes.
Dear Ms. Edith Bice,
Xarelto has no antidote. Warfarin, if overdosed with, can be counteracted with vitamin K. There are a few news stories of OD with Pradaxa, (dabigatran (Pradaxa)- and rivaroxaban (Xarelto)) and of death via bleeding out- because there is no antidote. Warfarin is a serious, dangerous drug (it’s rat poison), but if I had to chose, I’d pick it over Xarelto or Pradaxa. I hope this information is credible and helpful to you. New and improved isn’t always bad, but it isn’t that good in this case either. Not all drugs pushed and available from Pharma are bad, but some are very bad. FYI
I have a favorite concept I read from Hyperlipid blog -something like, if the cause of heart disease and heart attack was hypo-Lipitor-emia, the ‘cure’ would be to supplement with it. Some parts of modern medicine-pharma have run way off the rails.
First, great article. I’ve had absolute and relative risk hammered into my head many times at school, but this puts it together very well. I will definitely be sharing this with patients.
Also, your book Protein Power and Lifeplan helped inspire me to get into healthcare (and get healthy myself) about a decade ago. I’ve never forgotten your approach to health of the whole body, mind, and spirit while still hitting the literature to back it up.
Thank you so much for continuing dedication to health and the truth. I will bookmark and come back frequently!
Thanks for the kid words. Glad the program worked for you.
I see that your comment deadline is Jan 2, but your website was not working for 2 days (Apache error 80). So I hope you make an exception.
Dr. Eades, please help me interpret the following statement I’ve seen many times before, regarding A1c bloodsugar testing:
“For every 1% reduction in A1c, the risk of developing eye, kidney and nerve disease is reduced by 40%.”
(from this website: http://www.a1ctest.com/)
I think they are talking about relative risk here, right? But how can a 1% reduction become a 40% reduced risk? I don’t understand. Would you kindly explain? Thanks! Math is not my strong side 🙁
They are talking about a reduction of 1 percent as in from, say, 6 percent to 5 percent, which is really a lot more than a 1 percent reduction when you look at it percentage-wise. It’s actually about a 17 percent reduction. (1 divided by 6) And it’s a big reduction since, with those numbers, you would be going from abnormally high to mid-range normal. Blood sugar is probably more closely correlated with mortality than is cholesterol, so a major drop in HbA1c makes a big difference. You are correct. They are talking about relative risk, not absolute risk.
In your post on “The real cost of statins” you mentioned that statins use increased risk of diabetes mellitus by 2%.
A recent study by the Mayo Clinic entitled “Statin use and risk of diabetes mellitus in postmenopausal women in the Women’s Health Initiative” investigated the effect of statin use on 153,840 women without DM who were followed for an average of 6.5 years as of 2005. At baseline, 7.04% reported taking statin medication. There were 10,242 cases of self-reported DM. Statin use was associated with an increases risk of DM, hazard ratio 1.71. The association remained after adjusting for confounders, adjusted hazard ratio 1.48. (Pubmed 22231607)
By my calculations (and understanding):
Of the 153,840 women in the study, 6.65% of the the women developed DM
Among those not taking statins, 6.19% developed DM:
Among statins users, 10.58 % developed DM (6.19% x 1.71), which is an increase in absolute risk of 4.39%. (10.58% – 6.19%)
Among statin users, the increase in DM attributable to statins was 9.39% (6.19% x 1.48) which represents an increase in absolute risk of 3.20% (9.39% – 6.19%)
Am I correct in my interpretation?
The reason that the real increased risk of DM of 3.2% is higher than the 2% figure given the the post on “the real cost of statins” may be due to the longer duration of the study by the Mayo Clinic.
A recent study by the university of Manchester, UK ,noted that statin use is associated with reduced IGF availability which in turn is associated with diabetes. It was found that IGF1, IGF2 and IGFBP3 concentrations decreased following statin (atorvastatin) therapy. A differential effect of low- vs high-dose atorvastatin on IGFBP1 concentrations was observed with likely implications for IGF bioavailability. Thus it appears that the reduction in IGF availability resulting from statin use explains, at least in part, the observed increase in diabetes associated with statin use. (PMID: 23333902)
I’m not certain I follow your calculations, so I can’t comment. I don’t thinks the hazard ratio is calculated the way you think it is, but I’m not sure, because I don’t know exactly how you think it is calculated.
My doctor recently put me on Lipitor despite my reservations. My LDL is mostly small particles, so he said Lipitor is the best thing to prevent heart attacks. Heart attacks and high cholesterol run in the family, so I finally agreed to take the medicine. Are you saying that Lipitor won’t help after all? I know Lipitor can cause diabetes and other future ailments, and I would rather not take it, but my doctor made me feel like I didn’t have a choice.
I’m saying there is no conclusive evidence that statins work in any way for women. You need to discuss with your doc or find one who is more up to date on the statin medical literature. And, remember, you always have a choice.
I think this isn’t quite right:
“These ads weren’t technically misleading, but they didn’t tell the whole truth”
It should be:
“These ads weren’t technically false, but they didn’t tell the whole truth”
Because the ads pretty clearly WERE misleading, right? I mean that’s the whole point of this article. They misled people into thinking the risk reduction was more significant than it really is.
Yep. I agree with your version. They were technically misleading but not technically false.
Do you mind if I quote a few of your articles as long as I provide credit and sources back
to your site? My blog site is in the exact same area of interest
as yours and my users would definitely benefit from a lot of the information you present here.
Please let me know if this okay with you.
Regards!
Not at all. Go for it. Thanks for asking.
Hi Mike,
Was wondering if you had a comment on this video that was released today.
http://www.medscape.com/viewarticle/822145?nlid=52047_426&src=wnl_edit_medp_fmed&spon=34
Since the video isn’t available to everyone without going through the signup and login process, I’ve posted the transcript below.
If you’ve read any of my posts on statins or listened to any of my talks, you should be able to pretty easily guess my response.
Despite his lofty credentials, Dr. Veith is obviously not well versed in the medical literature, at least not the literature on statins. As I, and others, have pointed out countless times, statins do not confer any improvement in all-cause mortality in any group of people other than men under the age of 65 who have already had a heart attack. And even in that group, statins provide only slight improvement in all-cause mortality. The improvement is so slight that there is controversy in public health circles over whether or not it is worth the cost to provide this entire group with statins given the tiny minority who would actually receive benefit.
Dr. Veith is also completely in the dark as to the side effect incidence of these drugs.
I would say the witch hunt is more against those who dare to come out in opposition to statins as the experience after the Australian TV show proved.
Thanks for the comments. I’ve been reading your blog for some time, and posting a little, so yeah, I knew your take.
My impression (other than wondering who put Dr.Veith up to doing that) was the statin lobby seems to be somewhat desperate. Having a good grasp of the issue, I almost felt sorry for Dr.Veith. And do, if that’s what he really thinks.
It’s not the first, but that video seems to border on disinformation. I’m just amazed, and have been for years, at the control, lack of integrity, and manipulation of the information being pushed to doctors.
I just never get used to it.
~~~
Well!!
Since you wrote this article, I have attempted to find a robust way to convey the idea of absolute risk vs relative risk to my friends and family, but not very successfully.
I recently seem to have found an explanation that focuses on the simplest aspect of your argument above, and everyone finally seems to understand. I say: “It’s absolutely true that the statins provide a 36% reduction in risk of experiencing a heart attack or dying from heart disease, and don’t let anyone tell you different. If you’re willing to live with the side effects, it’s a pretty darned effective drug. But effective for WHO? Answer: For people who qualify for the study and have a crystal ball so that they know in advance that they will have a heart attack or die from heart disease.
“What’s that you say? You don’t own a crystal ball? (Or your medical profile wouldn’t have even placed you in the study?) Then the 36% figure has nothing to do with you.”
The listener then says: “Wait a second. You’re saying that the 36% only applies, after the fact, to the small fraction of the placebo group who will experience a heart attack or die from heart disease on the placebo and can magically know that in advance?!”
Say I: “Yes. That’s correct. For those unfortunate people, if they could buy a time machine and travel back in time to before they experienced the heart attack or died from heart disease, they would be a member of the group who would have had the 36% risk reduction on statins, and they would have good reason to consider reducing their risk by taking a statin.”
“But”, stammers the listener, “that’s ridiculous! There are no time machines! So how on earth could I know that in advance?”
Say I: “Exactly. To know the risk reduction that YOU personally would get from taking statins, you’d have to modify the 36% risk reduction that that group would have gotten from taking the statins, by also factoring in the chances that you’d even be in that group in the first place.”
“But”, stammers the listener, “there’s very little chance I’d even be in that group.”
Say I: “Now you’re getting it.”
In short: I stopped trying to explain the difference between relative risk and absolute risk, or to say that the relative risk is misleading.
Instead, I speak solely of the relative risk, applaud it for being 100% accurate, but point out that it’s only applicable to a group of people probably substantially different than the listener, and only practical in a magical universe where the listener can know in advance whether he just happens to be a member of that group.
Thanks Dr Eades!! I was a critical care nurse for 12 years before falling terribly ill in 2002, whereas I was akin to a 90 year old man with advanced alzheimer’s disease. (I was 34) I did not know my wife, nor 3 year old son, my parents nor my siblings. I was incontinent of bowel and bladder, could not feed myself, nor walk even with great assistance. I had an MRI showing multiple scattered lesions throughout the white and the grey mater, I had a brain biopsy revealing multiple autophagic vacuoles, an electron microscopy showing mitochondrial anomalies most similar to Mitochondrial Encephalomyopathy with Lactic Acidosis and Stroke Like Episodes (MELAS). I was headed to a nursing home pending bed availability, when I was examined by a visiting professor from Johns Hopkins, who suggested I begin a mitochondrial cocktail (12 vitamins, Amino Acids, and a robust dose of CoQ10), it was within 36 hours of starting this cocktail that I began to recognize my wife and family. I was able to answer simple questions, walk with assist, feed myself, verbalize the need to use the restroom, and I was discharged home 3 days later, diagnosed with “Viral Encephalitis” I clung on to this diagnosis, knowing Id be back to work soon. A few weeks after discharge, my wife and I watched Good Morning America, where Diane Sawyer was interviewing Dr Beatrice Golomb of the UCSD, they were discussing the Statin Effects Study Dr Golomb was to be starting. My wife pleaded with me to enroll, I replied, “Honey my job was to know everything there is to know about the drugs I gave, and there is no way Lipitor could have done this to me, it was a virus” for the sanctity of our marriage, I enrolled in the study, and when the study concluded, I received a phone call from Dr Golomb, who informed me that my case was not an isolated incident, and there were others with similar courses of illness, with similar test results. She referred our cases to who she referred to as, “one of the worlds foremost Mitochondrial Disease Experts” Dr Doug Wallace PhD, at UC Irvine, who opined that my use of Lipitor was the Causal Contributor to the Mito DNA mutations, and the Apoptosis. My jaw dropped as I thought of the hundreds of patients Id given these drugs to. I began to research for myself, critically analyzing everything, when I learned of Dr Duane Graveline, a former Family Physician and NASA Flight Surgeon. And from there, I have been devoting a good portion of my life, to educating people as to the dangers and Statistical Contortionism of these drugs, the absolute necessity of Cholesterol, and trying to wake people to the fact that we were not all born with a statin deficiency. I am in a facebook Statin Effects Group, in which was started about 14 months ago, there are now almost 1300 members from all over the globe. Most Statin Effects Sufferers, but there are 2 prominent cardiologists Dr Barbara Roberts who wrote “The Truth About Statins: Risks and Alternatives to Cholesterol Lowering Drugs” and Dr Aseem Malhotra of the UK, who is also an outspoken critic of these drugs. There are 3 Chemists, a few other MD’s, but mostly victims with a wide array of horrific effects. I welcome you or any of your readers to check it out http://www.facebook.com/groups/statins