I’ve posted on the health benefits of intermittent fasting (here and here) and on my thoughts on the inflammatory properties of food and overnutrition. These posts, particularly the one on inflammation, inspired a host of questions on whether intermittent fasting decreases inflammation. Based on my knowledge of the medical literature on inflammation and intermittent fasting I’m pretty sure that it does. A recent paper presents data indicating that it indeed does.
The April 2007 issue of Annals of Nutrition and Metabolism includes an article on the positive changes in inflammatory markers brought about by the intermittent fasting Muslims undergo during Ramadan.
As the authors put it in the introduction:
Intermittent fasting over a certain period of time is a feature of great religions all over the world and it is well known that nutritional habits, sleeping patterns and meal frequency have profound effects on maintaining human health. One of these fasting ceremonies is Ramadan. Ramadan is a religious month during which over one billion Muslims worldwide refrain from eating and drinking during the daylight hours for 1 month. The duration of restricted food and beverage intake is approximately 12 hr/day for 1 month, which makes Ramadan a model of prolonged intermittent fasting.
The authors are right in that Ramadan is a model of intermittent fasting with a host of subjects to pick from. I’m not sure that 12 hours of food abstinence a real intermittent fast makes, but it is a lot longer without food than the vast majority of us go for a month at a time. There is usually a pre-dawn meal that must be consumed before the sun rises and a post-fast meal that starts after sunset. I’m sure that Muslims don’t eat all night long during Ramadan, so I would venture that every 24 hours is made up of 12 hours without food, a few hours of eating before bedtime, sleep, then a meal in the pre-dawn hours. I would guess that there would be a total of maybe 5 hours during which people eat and 19 hours of each day in which they don’t. And for data gathering purposes, it’s nice that this schedule is maintained for an entire month. Since this fasting is a strong religious tenet for a group of people who take their religion very seriously, the data obtained from Ramadan fasting studies is probably much more valid than that obtained from typical volunteer subjects.
In this study 40 healthy, normal weight men and women aged between 20-39 years who underwent Ramadan fasting were compared with a group of 28 similarly aged men and women who did not fast. Data derived from questionnaires indicated that the majority of the fasting subjects ate their last meal between 1-2 AM and their first meal after the fast at around 6:30 PM, which means that most fasted for around 16 hours. (I assume that these subjects did not consume a predawn meal, eating late and preferring to sleep in instead.) The non-fasting subjects ate breakfast, lunch and dinner at regular times. Researchers collected twice-daily blood samples 1 week before Ramadan, during the last week of Ramadan, and 20 days after Ramadan.
Interestingly there was no difference in energy intake and no weight loss difference between the two groups. Apparently the fasters made up for lost time when they chowed down and ate as much as those who ate three squares throughout the day.
…average daily energy and water intake remained comparable in both the fasting and nonfasting group and the working hours of both groups did not change during the whole study. During Ramadan, in the fasting group, meals were taken exclusively at night while in the nonfasting group there was no change in the eating and sleeping habits. …the sleep pattern of the fasting group was delayed by approximately 2-3 h[ours] on average. The energy and the water balance seemed to be constant on a daily basis as the body weight and the 24-hour urinary volumes did not change during Ramadan. Hence there were two major changes in the routine of the fasting subjects: meal times and sleeping patterns.
What did the study show in terms of inflammatory response?
There were significant reductions in interleukin-6 (IL-6), C-reactive protein (CRP) and homocysteine during the fast that, in the case of IL-6 and CRP, lasted for at least 20 days beyond the fasting period.
What does this mean?
In short it means that the Ramadan intermittent fast brought about a significant decrease in inflammation.
IL-6 is a proinflammatory substance released by macrophages and other inflammatory cells that reaches the circulation and ultimately the liver. A number of studies have shown that about 30 percent of IL-6 comes from adipose tissue, especially abdominal or visceral adipose tissue (or more correctly, from the macrophages and other cells of the innate immune system that attack these fat cells). When IL-6 levels are high enough they stimulate the acute phase response in the liver. During the acute phase response the liver releases a number of proteins -including CRP- into the circulation. The job of these acute phase proteins is to prevent ongoing tissue damage, isolate and destroy the infective organism (or, in the case of visceral fat, the invasive organism) and activate the repair processes necessary to restore normal function. CRP is an acute phase protein that binds to certain sites on microbes, probably assists in the helping other parts of the immune system attack foreign and damaged cells, and enhances the consumption of these cells by the macrophages. CRP is an important player in the innate immune response, which is the blind, hardwired early responding part of our immune system.
Both IL-6 and CRP are elevated during inflammation, and both, but particularly CRP, are used as markers for inflammation. There is now a large amount of data showing that elevated CRP levels are a potent risk factor for cardiovascular disease.
The decreased levels of homocsyteine during fasting are an intriguing phenomenon. Homocysteine can react spontaneously with many biologically important molecules, especially proteins. It can react with and cause damage to the folding of important proteins, i.e., enzymes, immune proteins, receptors, growth factors, and structural proteins, leaving them with a configuration that is less than optimally functional. High homocysteine levels cause oxidative damage and are thought to cause inflammation, especially in the endothelium. As a consequence, elevated homocysteine levels are, like CRP, a fairly potent risk factor for cardiovascular disease.
Homocysteine is an intermediary in the metabolic pathway between methionine and cysteine, both important amino acids. Folate and vitamin B12 are essential in making the transition from methionine to cysteine without allowing large amounts of homocysteine to stack up. A deficiency of either folate or vitamin B12 (both B vitamins) allows an increase of homocysteine, which makes it’s way into the circulation and causes problems. What makes this study so interesting is that both folate and vitamin B12 levels increased substantially in the fasting subjects despite their not eating any more food containing these substances than the nonfasting subjects. It’s this increase of the folate and B12 that more than likely decreased the levels of homocysteine in the fasting subjects.
The authors speculate:
…both folate and vitamin B12 levels were increased in the last week of Ramadan in the fasting subjects and a negative correlation has been detected between these two vitamins and homocysteine levels. None of our subjects used any kind of vitamin supplements and according to the questionnaire, consumption of food containing B vitamins did not change during the whole study period. The changes in the rest-activity cycle and meal schedule during Ramadan may beneficially affect the bioavailability or redistribution of cofactors like B vitamins in the methionine pathway, which in return may lower plasma homocysteine levels. These results are consistent with [a] previous study in which homocysteine levels but not B vitamins were evaluated in the fasting subjects during Ramadan.
This ‘bioavailability’ and/or ‘redistribution’ is similar to that which happens with vitamin C during an all-meat diet. It is well known among arctic explorers that those on diets of nothing but fresh meat don’t get scurvy. The British sailors in the 1700s who were afflicted with scurvy consumed a diet composed primarily of carbohydrates. When British naval surgeon James Lind gave them fresh lime juice their scurvy was cured or prevented. As we all know now, the cure and prevention came about due to the vitamin C in the lime juice. Most researchers and physicians still believe that diets deficient in vitamin C will cause scurvy, but this isn’t the case, especially with fresh meat diets. The glucose molecule competes with the vitamin C molecule for entry into the cells. When glucose molecules are high – as they are in high-carb diets – much more vitamin C is required to compete with the glucose and actually make it into the cells. During all-meat diets, glucose is low, and a much smaller amount of vitamin C can still enter the cells and do its job.
Whatever the case, fasting reduces the levels of homocysteine, which is a very good thing.
Below are the charts showing the reduction of IL-6, CRP and homocysteine in the fasting subjects.

IL-6 Males

IL-6 Females

CRP Males

CRP Females

Homocysteine Males
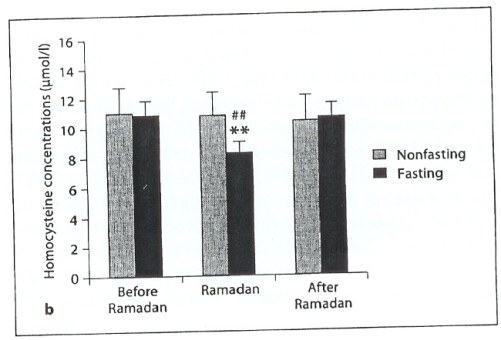
Homocysteine Females
This study adds to the data showing that intermittent fasting does indeed reduce inflammation. Whether the reduction comes from the long period without food or from the change in sleep patterns the study doesn’t show. But I think it’s reasonable to assume that it is probably the former rather than the latter. Reduction in sleep time all by itself has been shown to be inflammatory, so I would guess that were these subjects to have maintained their regular sleep patterns and fasted fasted, they would have shown an even greater decrease in inflammatory parameters. But that is speculation; we’ll have to wait for the real data.
This paper confirms for me the idea of not eating between meals and not consistently snacking as some would recommend. I like to let things rest totally between meals and not nibble, even on low-carb snacks. Based on the intermittent fasting data that is rapidly accumulating, I think that eating as infrequently as possible is probably the best bet to keep your innate immune system behaving as it should, especially if you follow a higher-carb diet.

Dr. Mike,
Thanks for posting this, which for me was coincidentally incredibly timely. A few weeks ago, I determined that, in an attempt to improve even further on my type 2 diabetes control (my last two a1c tests have been under 6%), it was time to go for it and do some IF. I made a slight modification of your proposed schedule that essentially gave me three 22-hour fasts and one 18-hour fast per week.
I stayed on this for about two weeks and other than sometimes feeling “hungry” — I’m not convinced yet how much of that was actually psychosomatic, to be honest; there was no grumbling of stomach or whatever — I honestly felt pretty well, a headache or two notwithstanding, as I am highly prone to them anyway. My blood sugar was normal (by which I mean low 80s) whenever I tested, which was never post-prandial (I was short on strips) but even so. However, not always eating when the family did started to wear on me, as did the notion that I was hungry, so then I decided to try a modification whereby I just didn’t eat between dinnertime and lunch the next day (sort of the “look I’m in high school again” diet, I suppose.) In theory that’s a 16 hour fast every day, more or less.
Interestingly, I found it very difficult to maintain what on face value was a simpler plan. The urge to eat off schedule if anything increased, and once the slipping started, the blood glucose came up, and by Friday, I couldn’t get my fasting below 100 and frankly I felt like crap. Not good. So Sunday I got back on my original plan. That’s yesterday, mind you, following some mid-afternoon snacking. That was it until breakfast today, and then I’ve been off again since lunch and will be until lunch tomorrow. And lo and behold, a few hours ago I tested (probably 5 hours after lunch?) and I was back down to 81 mg/dL.
Do I feel the lack of food? Yes, absolutely, and I expected to after the past week of slacking. But I’ll get over it. The normalized blood sugars are just too tempting. And iced tea and coffee are my anti-food. 🙂
Anyway, I’d actually seen the Ramadan study when googling around about IF recently, and thank you again for this timely discussion of it. I hope this utterly anecdotal and not very scientific personal story is useful in some way, or at least a decent read. I’ll be watching for more discussion of IF!
Oh, before I go, my weekly schedule:
8am Mon – 2pm Mon NO FAST
2pm Mon – noon Tue FAST (22hr)
noon Tue – 2pm Wed NO FAST
2pm Wed – noon Thu FAST (22hr)
noon Thu – 2pm Fri NO FAST
2pm Fri – noon Sat FAST (22hr)
noon Sat – 2pm Sun NO FAST
2pm Sun – 8am Mon FAST (18hr)
Cheers,
R
Hi R–
Thanks for the interesting story. When you tried your look-I’m-in-high-school-again approach, did you eat low-carb or did you follow the see food diet? (That’s the I see food I eat it diet)
Glad to hear your blood sugars have come back into line.
Cheers–
MRE
This is very interesting. I’ve read your other posts about fasting and I am wondering about your thoughts on the subject of our lean tissue and organs not being able to store protein, and therefore fasting causing muscle catabolism (and subsequent slowing of metabolism–like on a low protein diet)?
1 lb of muscle = approx. 37 calories burned to maintain it/day
Hi Alex–
Nothing really stores protein except for muscle and connective tissue. There are protein structures in all the cells, but they aren’t really storage structures like glycogen is for glucose. As long as protein intake is sufficient on eating days, I don’t think intermittent fasting will slow down metabolism.
Cheers–
MRE
Thanks for another interesting IF post.
Could you comment on studies that (purport to) show that children perform better in school when they eat breakfast compared to when they do not? Are the studies well done? Has anyone tested the effects of IF on the mental performance of either adults or children?
Thanks,
Jessica
Hi Jessica–
Due to the fact that they’re growing, I’m not sure that an intermittent fast would be ideal for children. Kid’s probably will do better with a good protein breakfast as compared to not eating breakfast or eating the typical high-carb cereal or, God help us, Pop Tart breakfast.
I haven’t seen a paper on mental performance with IF (that doesn’t mean there isn’t one; it just means that I haven’t seen one). But a number of papers have shown that BDNF increases with IF and doesn’t change with caloric restriction. BDNF (brain-derived neurotrophic factor) is the substance that the brain secretes to grow new brain cells.
Cheers–
MRE
Why do you think that conventional wisdom tells us not to skip breakfast (to avoid weight gain), and to “graze” or consume many small meals/snacks throughout the day? Does it have to do with insulin and blood sugar control differences between high vs. low carb eaters, or is there something else I am missing? While I no longer eat high carb, I do still snack frequently, and wonder if I need to change this habit? Secondly, I am interested in IF, but wonder if the regularity of simply delaying the morning meal to achieve a 16 hour fast is really being true to the spirit of “intermittent”? Thanks for all of the great information!
Rod
Hi Rod–
I think the conventional wisdom arose around people eating conventional (read: high-carb) diets. In terms of keeping blood sugar and insulin levels more stable during a high-carb diet, it probably is better to divide that diet into small snack-sized portions that are consumed throughout the day. If, on the other hand, you’re eating low-carb, I don’t think it makes as much difference, since your blood sugar and insulin levels are going to be much more in control anyway.
And I do think delaying the morning meal to a time that will result in a 16 hour fast is being true to the spirit of IF. No one knows what the optimal amount of time spent not eating to gain maximal effect, but I would say that any time spent in delaying eating is beneficial.
Cheers–
MRE
I don’t think intermittent fasting will slow down metabolism.
Is there any hard science on that particular point, Doc? When I explain my RC via LC and IF to friends and family, I nearly always get the “fasting shuts down your metabolism” line.
Thanks!
Hi John–
No, there’s no hard science on this. In fact, there is really no hard, hard science on metabolic rate. Numerous studies show that different people of the same weight eating the same amount have differing metabolic rates while people of differing weights and differing diets have the same metabolic rate. About the best one can say (which I often do) based on the data at hand is that the best measure of metabolic rate is weight, even though that’s not all that accurate.
Cheers–
MRE
this is great stuff, thanks! I started a fasting plan called fast5 just over three weeks ago. You choose a five hour window and only eat during those hours-so it’s a 19 hour fast. I still get pretty damn hungry as my eating window nears, but so far I’ve been able to manage it. Lost 5 pounds too!
your new article should keep me motivated for awhile, thanks again
Glad to hear you’re re-inspired.
Cheers–
MRE
Hi Dr Eades. Thanks for writing about IF. After almost a year of IF being on my ‘to-do’ list for ‘some day when I grow up and stop being a hedonist’, I’ve decided to sacrifice the cream in my morning coffee and one meal a day, to officially be IFing. The meal I skip is the one where I’m standing in the kitchen before bed, getting a tan from the fridge light, noshing on bologna and cheese, when I know darn well I’m not really hungry.
I don’t expect many changes, since I’m used to only eating two main meals per day and exercising on an empty stomach, but I’ll drop a line in a while to let you and other readers know my results.
Cheers!
Kristine J.
Hi Kristine–
I’ll be curious to hear your results myself.
Cheers–
MRE
I’ve stuck (and continue to stick) to low carb in all cases; in fact I tend to be pretty tight about it, since Dr. Bernstein’s book got me started in this direction — like him, I tend to stay under 30g/day. Having said that, I wouldn’t be upset if increased insulin sensitivity were to let me relax that a little bit somewhere down the line. (Of course, I can’t see ever consuming as much carbs as I was told to by a nutritionist after my diabetes diagnosis. But that’s another rant.)
Thanks for posting this. I’ve been IFing since your initial post (at least a 15hr fast each day, no set schedule other than that) and lowcarbing since May 2006. I found out I have food intolerances as well, and have been gluten, casein and (mostly) soy free since October 2006. Lowcarbing/tolerant foods got rid of all my prior symptoms (and they were legion) but one – chronic bloating/abdominal distention. I just always looked preggers!
Since IFing, my belly has deflated…finally. Never thought I’d be rid of the thing. And I’ve lost that overall puffy look. People think I’ve lost way more weight than I actually have.
Thanks for all your work on the subject! It’s appreciated.
Hi Tracy–
I’m glad to hear you’ve done so well. Keep it up.
Cheers–
MRE
Thanks Mike, as usual.
Aside from homocysteine, I think Jeff Volek (and I believe others as well) has also shown significant improvement in inflammatory markers not by fasting but by significantly reducing carbohydrate intake. I don’t particularly favor the idea of the ‘very-low’ carbohydrate approach that he has used (only because for the majority of us, adherence to those very low levels on a daily basis may not necessarily happen). Nonetheless, significant reduction in carbohydrate intake also improves inflammatory markers. Some speculate that it is because weight loss (i.e. fat loss), regardless of how that is achieved, I’m inclined to believe that it is the reduction in carbohydrate intake what works as an underlying factor.
In any case, my point is that since not everybody is up to fasting, another good way to improve inflammatory factors is plain good old carbohydrate reduction (plus a tweak here and there with omega-3 fat intake to counterbalance any excess of omega-6 fats in the diet). Or, perhaps like you and MD have done, fasting but keeping a low-carb approach when it’s time to eat. Just my $0.02.
Cheers-
Hi Gabe–
I tend to agree with you that low-carb dieting reduces inflammation. But as I recall from a couple of Volek’s talks I attended he attributes the decrease in inflammatory markers to the weight lost, not specifically the low-carb diet.
I also agree that not everyone is up to fasting – I’m not myself all the time. But there are a group of people who do well and don’t mind the deprivation of the fasting days. It does make life a lot easier not to have to worry about eating half the time.
Your $0.02 is always welcome.
Cheers–
Mike
Dr. Eades
Thanks so much for posting this and keeping up with this area of research. I’m on day 180 of a regular 18-20 hour daily fast. I eat dinner every day for an hour or two and then fast until the next day dinner. I have eaten lunch about 10 times during this period. I eat LC all the time. I’ve been introducing this concept to hubby who has joined me in this “intermittently”. He’s just finished losing his weight through LC and we’re developing an ongoing maintenance plan.
In the past 18 months, I’ve lost 100 pounds eating LC and adding in exercise. I added in IF in the past six months and have seen remarkable additional fat loss–my body fat is about 17-18 percent now and I’m a very healthy 47 year old woman.
My only remaining question in this lifestyle is whether taking supplements (particularly the oils which may contain a few calories each) technically breaks the fast. I know you and MD continued to take your supplements on your regular schedule. Do you continue to hold this view? Is it more beneficial to have the supplements spread out to assist with absorption or is it better to take them all at once in order to protect the fast?
Many of us on another forum are eager to hear your responses in this regard.
Again, just delighted to see your ongoing posts and really value the insight you give us daily.
KB
Hi Kathy–
First, let me congratulate you on a remarkable job. Not many people lose over 100 pounds to reach a body fat percentage such as yours. I have nothing but admiration.
I don’t have any data to back me up on this, but I don’t really think it makes much of a difference when you take the supplements as it relates to the fast. The tiny number of calories consumed won’t – in my opinion – matter a whit. I would take them when convenient.
I’ll keep my eyes open for any studies that address this specific issue and pass along the info if and when I get it.
Once again, great job! Keep after it.
Cheers–
MRE
Thanks for the input Mike–I’ll pass it along.
KB
LabCorp has a CRP reference range(adjusted to mg/dl)of 0-.3.
I was surprised by the male “Before Ramadan” CRP of about .4. Would an average of .4 be unusual for fairly young US males with BMI
Hi Dave–
CRP normal ranges vary by lab. In some any amount below 10 mg/dl is considered normal.
Cheers–
MRE
The internet lost the end of my post. My fat fingers – probably.
… with BMI
I think it lost it again.
I figured it out. If I use the “less than” sign, the computer thinks I mean to use HTML. Sorry.
No problem, but I still don’t have the end of your post. I think I know what you were saying anyway.
I’ve been chewing on this IF concept ever since you brought it up, especially since I even though I am at a mostly ok weight (5’4″, +/-126#, 45 yo), I have an impaired glucose metabolism (fairly normal glucose levels and 5.5% A1c with constant LC, but diabetic levels with 3hr GTT and HC food challenges).
But I think what is holding me back from trying IF is how to best fit it in with family life & children. I have a grade school child (without making a big deal about it I keep his carb consumption moderated quite a bit when I can because I had gestational diabetes with him, which raises his risk factors) and I am not sure how a different timing of my meals would impact on him (as a role model, the family cook, etc.). I guess if I just ate dinner with the family it would be less of an impact, as my breakfasts and lunches are often on my own. But evenings are full enough now, I can’t imagine eating more food at dinner or a second dinner to make up for fasting through breakfast and lunch.
Managing a household and rearing a young boy requires a certain amount of energy throughout the day, and I often don’t have enough energy as it is so it is hard to think of not eating in the day and not pooping out. Currently I find if I haven’t eaten breakfast or lunch I am quite crabby and tired by afterschool – – not a good thing during son’s homework time.
My husband eats LC, too, but I’m not sure how he will react to IF. He needs to go to lunches and dinners with colleagues so I doubt he will join me in IF.
Away from home I anticipate other issues, largely social. I can stay LC when ordering in restaurants and eating at friends’ houses (I don’t count carbs at all but I can usually guestimate if I don’t eat obvious HC foods), but I guess I am less confident about the social issues when I’m a guest of distant friends and relatives, especially the European ones, who already make disparaging comments on “Americans and their special diets and food fetishes” (I try to be inconspicious with LC in someone’s home, but some notice and ask). I’ve been more direct about my LC needs since the glucose impairment confirmation, but I don’t necessarily want to discuss a yet another even more unconventional eating style when it becomes apparent, ya know?
BTW, I notice your response rate is creaping back up lately. Sort of like those sneaky carbs, eh? I don’t expect a response, but future posts about blending IF with family life, social situations, traveling, being a guest, etc. are always welcome.
Cheers,
Anna
Hi Anna–
It’s tough fitting it in with social occasions that demand eating. That’s one of the reasons MD and I sort of fell away from IFing. It was much easier than we both expected it to be, but it seemed that with our hectic schedule we always ended up at some function where eating was in play. We would try to figure days in advance how to schedule our fast so that these events would fall on eating evenings, but it never seemed to work out.
Let me know if you give it a whirl.
Cheers–
MRE
Dr. Mike.
I got my lab results after following the PPLP for 5 months. I lost 30 lbs. I lift weights 3x /week. My trig. went from 197 to 88. My total Tot. CHol stayed about the same–265 (the Dr. wants to put me in statins), the same for my LDL~200. My HDL went up slightly–to 43 from 37. My fasting blood glucose went from 128 to 114. My Hg1Ac was 5.6%. I am very pleased with the results. But I am still concerned that my FG is still > 99. Will I see an improvement with more time? I adhere to the PPLP at least 95% of the time. If a carb binge (not very often) I immediately get on intervention level. I can thank you enough for the great service you provide via this blog.
Hi zeledoc–
I’m pleased to hear that you’ve done so well. It would guess that your FG would go down with time as you continue to follow the program and re-establish your insulin sensitivity.
Keep me posted.
Cheers–
MRE
Wow, great stuff! I was just contemplating a cheaters fast (Mediclear or Ultraclear), so this was very timely. I have always had a big problem with fasting myself because my blood sugar swings would make me unbearable. I was wondering what your thoughts on using glutamine or maybe some free form aminos to try to keep me from wanting to chew my arm off. Anything to try and promote the ketogenic, the sugar burning pathways are very hungry buggers.
Hi Robert–
If you want to try free form amino acids, I would go for the branched-chain amino acids, leucine in particular. Luecine is intimately involved – probably more so than any other AA – in the gluconeogenesis process.
Cheers–
MRE
One thing I’ve been reading about lately is how lectins keep us from absorbing and utilizing vitamins and keep the intestinal epithelial from healing. I wonder if perhaps the lectins in the grains and beans people are eating is causing some of the issue with the B vitamins. Our intestinal flora is supposed to be able to produce B12 from what I recall. Maybe a break from that constant bombardment of lectins is what is helping the fasting Muslims.
Here’s an article I spied in Science Daily recently about lectins damaging the intestines. http://www.sciencedaily.com/releases/2007/08/070801091240.htm
All I know is that since I stopped eating grains and dairy products my autoimmune arthritis (ankylosing spondylitis) is vastly better. I had been low-carb but having flares until I gave up the low carb products like low-carb bread and wraps.
My IL-6 and CRP are under lab ranges too. Interestingly a lot of AS patients find a “No Starch Diet” relieves a lot of pain and fusing.
You are right on the money, Nancy.
Some lectins are not harmful – tomato lectins, for example. Others such as WGA (wheat gluten antigen) are really damaging to the bowel lining. Going grainless for a day allows the lining to heal and ready itself for another assault the next day. During everyday eating of grains, the damage in susceptible people never heals.
I’m very grateful for this blog, Dr. Eades – as, I’m sure, are many others.
Thanks. I’ll keep giving it my best.
At the risk of overcommenting on this thread, Kristine’s comment earlier made me wonder — is it a big hit to the value of IF to go ahead with a splash of cream in your morning coffee? If so, I may be in trouble. 🙂
Probably not a big risk, just don’t get carried away.
Hi there!
I so look forward to your blog entries! It is a real education and a pleasure to read a blog with some substance!
Your entry here about IF makes me think of a book I had read and followed for a couple of months called: “The Warrior Diet”. Are you familiar with that? I was hoping to get your thoughts.
I tried it, as I say, eating only once a day, but gained a huge amount of weight. Looking back now, I knew nothing of the impact of high carb eating and so that was probably my downfall.
Here is the author’s blog.
http://www.warriordiet.com/blog/
Perhaps this isn’t the place to ask you this, but what is your thought about his accusations that pork is “an estrogen drug” and that turkey shouldn’t be eaten?
It does get confusing when you read people that sound very authoritative give opposite opinions!
I have come to trust yours though!
Thanks for good work!
Hi Bruce–
Thanks for the kind words and the vote of confidence.
I do not believe that pork is “an estrogen drug” nor do I think turkey should be avoided. When I hear stuff like that my index of suspicion that whoever said it is an idiot goes screaming upward. I would love to see any scientific data to back those statements up, but I’m pretty sure none exists. If anyone out there has such a scientific paper please send it my way, and I’ll eat my words.
Cheers–
MRE
Another interesting post especially on the vitamin ‘bioavailability’. I’ve been IFing since you first blogged about it last year but on a random basis – a couple of days a week and also a week or so out of every five where I only eat one good meal a day. Could that explain why my B12 levels came in at nearly double the high end of average after a recent test – 1557 ng/L? (liver damage and haematological malignancy was ruled out). My vitamin C and vitamin D also came in at the high end of average FWIW. These days the only supplements I take are magnesium.
Hi Zedgirl–
I suppose it could explain the increased B12 you experienced. The paper this post was about was the first time I had seen that mentioned. I have no idea what the mechanism is, and neither do the authors I suspect. But, hey, it’s a good thing. Low-carbing and IFing are full of surprises.
Cheers–
MRE
Thank you so much for the excellent review of the Ramadan study! I have been using The fast-5 method and really enjoying it. I do like to see research that backs up the system. I am a medical student and constantly have attendings telling me I shouldn’t skip meals! They are always eating something like granola bars or nuts between patients. I like to have good studies to back up my approach to eating.
I was wondering if you had looked at the following study. It seems to show a mix of good and not so good results. I was concerned about the elevation in blood pressure. What is your take?
Results: Subjects who completed the study maintained their body
weight within 2 kg of their initial weight throughout the 6-mo period.
There were no significant effects of meal frequency on heart rate,
body temperature, or most of the blood variables measured. However,
when consuming 1 meal/d, subjects had a significant increase
in hunger; a significant modification of body composition, including
reductions in fat mass; significant increases in blood pressure and in
total, LDL-, and HDL-cholesterol concentrations; and a significant
decrease in concentrations of cortisol.
Conclusions: Normal-weight subjects are able to comply with a 1
meal/d diet. When meal frequency is decreased without a reduction
in overall calorie intake, modest changes occur in body composition,
some cardiovascular disease risk factors, and hematologic variables.
Diurnal variations may affect outcomes. Am J Clin Nutr 2007;
85:981– 8
Thank you again for your wonderful reviews/ideas!
-Daniel Cote
Hi Daniel–
I finally pulled the study to which you referred only to find that I had already read it. I wouldn’t worry too much about the changes in blood pressure: they were minor to say the least. I don’t know why the BP went up in the study group. In virtually all other papers I’ve read, BP goes down with intermittent fasting, which makes sense when you think about it. In this study, LDL went up a little as well, but there is a rationale for that. Since triglycerides went down and HDL went up, it’s pretty clear that the LDL pattern shifted from a smaller, denser particle size to a larger, fluffier one, which is a good thing. And in this study, cortisol levels dropped markedly with the shift to once daily eating. Anything that drops cortisol levels is good. So, all in all, I believe this study does nothing but bolster the idea that longer intervals between meals and/or skipping meals is a more healthful approach to eating, especially if what you want is a higher carb diet. Both diets in this study contained about 50 percent carbs.
Cheers–
MRE
Mike the more I read on Low-Carb paleo type nutrition the more interesting it becomes. I have been LC for about 7 yrs now and am doing very well.Initially went from 110kg to 78kg over the first year and have been stable since then. When you brought up your initial post on IF I decided to try it out. What I did was to mentally put myself into what I imagined to be a primitive hunter-gatherer society. I applied my hunting experience and realised that it is probably illogical to get up in the morning and prepare a meal before you head out hunting. The best time to hunt is that period of time when dawn approaches. It was probably a relatively safe time to hunt for paleo man as hopefully the major predators will already have killed and it also means that you have the daylight hours to process and carry your kill back to your “cave”. I can imagine that you might eat a little in the field but most of your food would be consumed back home in relative safety around the fire in the evening. So now I don’t eat breakfast most of the week. I might have a brunch one day in the weekend. Lunches are normally very light. Some meat and a kiwi. In the evening I prepare a feast and eat heaps usually finished by 7:00pm. I probably never exceed 40ecg in a day. The results! Well over the last three months I have lost a further stubborn 6kg. I don’t get hungry and tend to eat lunch after 1pm. I’m 58 now and this is the best I’ve felt in 30yrs.
Look forward to your articles.
Cheers: John
Hi John–
I’m happy to hear you’ve done so well. Thanks for your dietary history; maybe it will be an inspiration to others.
Cheers–
MRE
Linoleic acid is supposed to be inflammatory right?
I was reading an old metabolic study here:
http://www.ajcn.org/cgi/content/abstract/26/2/197
In it they fed people nearly 7000 calories worth of corn oil per day and they barely gained weight. Even more surprising is that oleic and linoleic acids appeared to have different effects. Whats going on?
The study also mentioned participants feeling warm after a high intake of fat. I think that proves your theory of futile cycling.
Hi Freddy–
Yes, linoleic acid is inflammatory in large doses.
The warmth the study mentioned does come from futile cycling. This paper was obviously written by someone for whom English is not a first language. I had a little difficulty the first time through understanding exactly what was going on. I’ll print it and read it more carefully to see if I can tell what they’re trying to say.
Thanks for sending the link.
Cheers–
MRE
I’d like to join you, Mike, in congratulating Kathy B’s amazing journey, and perhaps just offer one last penny for the night 🙂
In her comment, I couldn’t help but revisit the ‘calorie issue’. Since I think it’s been shown more than enough times that calories are not ‘created equal’, her question about supplements, specifically oils, technically breaking the fasting could plausibly be addressed from a different angle. I think that the reason such supplements wouldn’t make a whit of difference is because her now very well conditioned metabolism. In other words, oily supplements (which could seemingly be thought as highly caloric) won’t be treated in the same way now than when she started her low-carb journey, and I would speculate that not even occasional high-carb meals would either, as long as it’s an occasional occurrence. Her body is better able to handle caloric intake as well as carbohydrate, a common result after a period of carbohydrate control.
Since I seem to have a knack to ‘overthink’ certain things, I can even conceive a different type of fast, which doesn’t necessarily mean lack of eating, but lack of eating the stuff that makes your metabolism react in the wrong way.
Today, for example, as it has happened several times, I was craving for some nice hamburger patty. I know, some people think is crazy to crave for meat. I treated myself with two juicy and rather big patties, cooked to perfection, which I placed on top of more or less one and a half cup of mixed lettuce types. Between the salad and the patties, there was a layer of feta cheese and the meat was topped with a slice of mild cheddar. Needless to say that the amount of protein for lunch was quite a lot more than what I’ve estimated my minimum protein intake. Result: not hungry at all for the rest of the day; not feeling deprived in any way. In terms of calories, a dietitian would probably get on my case because it would seemingly be too little, though if you think of the size of those patties and the cheeses, I don’t think I faired too low in the calorie department. However, the effect on my metabolism is anything but detrimental. I could conceivably propose this as a kind of fast, especially if I eat until I feel hungry, not because I’m imposing a schedule for food intake and food deprivation, but because the dynamic action of the amount of protein I eat is working its physiological magic: increasing satiety and for longer periods while providing what my body really needs. Who knows, perhaps the paleolithic man went through something similar, especially after consuming that large prey, which kept them satieted, therefore inducing a reduction in food intake until the next hunt.
Had I chose a different composition of those calories, mainly with less protein, the result would have been very different in terms of satiety, as I have also experienced myself countless times.
Perhaps there is room to redefine what fasting is, beyond the total absence of food intake, but more in terms of intake of the bare minimum that the body needs.
Cheers-
Hi Gabe–
I think you’re exactly correct in terms of what the low-carb diet does, but I do think there is metabolic good to be had simply by going without food – even low-carb food – for a period of time now and then. That’s why I like to go as long as I can between meals and even skip meals frequently.
Cheers–
Mike
IF is sweet. I’m currently IF-ing Ramadan style for about 16 hours 2 meals @11Am&6:30PM each day. The local imam would probably have a problem with the way I worded the previous phrase but I kind of dig it. This seems to slash my insulin needs once again. I think if I were to begin an exercise regimen I coud be down to the single digits for daily insulin requirements, which is sweet for a Type 1. My one concern is that I now eat two larger meals of about 750+ calories and am wondering if this could negate the effects of IF-ing at all.
Hi Neal–
I don’t think the larger meals with negate the effects of the IF. That’s the whole point of IFing: to not eat for a long period, then to eat what you want. If you’re eating only two meals per day at 750 calories each, that adds up to only 1500 calories per day, which ain’t all that much.
Cheers–
MRE
Thank you Dr Eades. I’ve been reading your blog for over a year now and I must say that you are amazing in the way you keep up your readers’ comments and also in the very professional approach you take in expressing your opinions.
Regarding this study, one thing I suppose one can extract is that inflammation markers can be improved without having to go through extreme fasting. Maybe skipping breakfast is enough.
Personally, I’ve followed a low carb approach with occasional fasting lasting from as short as 10 hours to as long as 22 hours. I can’t say if this has done anything to my body but the fasting is really easy for me. I don’t feel deprived. In fact I feel invigorated and relieved from having to eat at a certain time.
Thank you for this great site and I hope you keep us informed and entertained.
MT
Hi Mike–
Thanks for the kind words about the blog.
I think that probably anytime spent not eating is good. If you skip lunch, that’s not really an IF, but I would bet that you get benefit from it. For that reason I try to eat when I feel hungry irrespective of when that is. I often go until mid or late afternoon before I notice that I’m a little hungry – other times it’s earlier.
I’m glad you’re doing so well.
Cheers–
MRE
I’m on a very low-carb diet (used to be no carbs, I shall go back on that route once my summer job ends and classes begin again, it’s hard when you work all day to get a diet high in caloric while still cutting all carbs; my carbs mostly come from a very high fat yogurt which is particularly good for my digestion).
I never feel deprived when I fast. I can go very long time without eating. I remember once when I ate at about 10AM one day, had a lot of classes the other day and the last one ended at about 6PM, put a whole chicken in the oven once I arrived home (covered with a lot of duck fat), I went to the gym and had a very good workout, and only ate right after at around 8 PM.
It seems that weight training in the morning kills my appetite even more, I heard it’s from the blood going to the muscles rather than staying around the digestive system.
Anyway, very low-carb and intermittent fasting go hand-in-hand and I would consider it the natural way to go. I have to go!
Hey Max–
Thanks for the dietary history. I’m glad you’re doing so well.
Cheers–
MRE
Just wondering what your views are regarding acceptable drinks to consume whilst fasting:
E.g.
Black/White Coffee/Tea (without sweetener)
Green Tea (straight)
Water
Milk
Alcohol
Thanks,
Dan
Hi Dan–
During the fasting days any beverage that is non-caloric is probably okay. That would include coffee and tea (unsweatened), diet drinks, water, and sparlkling water. If you drink liquids with calories – milk, for example – it’s not really a fast.
Cheers–
MRE
You said: “For that reason I try to eat when I feel hungry irrespective of when that is. I often go until mid or late afternoon before I notice that I’m a little hungry – other times it’s earlier.”
This is where I’ve found myself gravitating, despite my big talk about schedule. And actually, I’m at peace about it — putting a little trust in my body. (On the other hand, I do not trust my body to tell me when to STOP eating, because that’s never worked well for me, almost certainly because I tend to eat awfully fast.) The best part is that it makes sense to others, too. “Well, I’m not having supper because I’m not hungry.”
I eat fast as well. I’m working on slowing down, taking my time, not gobbling my meals, etc. If you do this it let’s cholecystikinin and the other gut peptides that feed back on the hypothalamus giving the you’re-getting-full signal time to work.
Dear Dr Eades,
Thank you for the posts on inflammation and in particular IF. The advice from nutritionists and others regarding regular eating patterns has never sat well with me and now there is light!
As I was reading your post on Ramadan, a question was forming in my mind regarding supplements. As a type II diabetic who has declined to take the Metformin and statins, I take a range of vitamins and minerals to help combat the disease.
I have always though (and I believe this is widely recommended) that it is best to take supplements with food so that the assimilation is more efficient.
Could you comment on how supplementation sits with intermittent fasting? As the fasting itself is largely responsible for a considerable list of potential benefits, does this make supplementation partly or even wholly redundant?
Or should supplementation follow the fasting regime? For example, take no supplements during the fasting phase but continue them in the eating phase?
I look forward to your future posts which are always extremely informative and helpful in this crazy world of conflicting and misleading information from agencies and companies with vested interests.
Best wishes
Barry Dench
(In the uk)
Hi Barry–
I don’t know which supplements you are taking, but some supplements – the fat soluble ones, which include CoQ10, carotenoids and other similar antioxidants – are fat soluble and won’t be absorbed if not taken with a meal containing fat. It’s not a problem on eating days because you simply take your supplements with your meals. When I IF I take my supplements (when I think of it – I’m a bad regular pill taker) on fast days I always include a couple of fish oil and krill oil capsules, which provide the needed fat. I also take a type of CoQ10 that is dissolves in the mouth and is absorbed directly through the oral mucosa.
Having said all that, I would imagine that it wouldn’t hurt to avoid the supplements during fasting days. The fast is probably going to do more good for the diabetic condition than all the supplements in the world. If I were going to list my top five supplements for type II diabetes they would be magnesium, lipoic acid, CoQ10, biotin, and carnitine. I hope those are a part of your list.
Best–
MRE
This may be a way dumb question to ask, but since I have dealing with the cold/flu (don’t ask how I managed to pick that up in the middle of August). Since fasting reduces inflammation, is that why we lose are appetite so quickly when we’re sick? I’ve noticed since I’ve been sick this weekend, I’ve been eating maybe twice a day, and even then it’s a fraction of what I’d normally consume at a meal. Is that due to your body trying to reduce inflammation, or is that because your body is not able to process as much food, since the digestion process is so energy consuming?
Hi Noah–
I suspect it’s because the body is trying to conserve its reserves for infection fighting. Digestion consumes a lot of band width, and by slacking back, the available energy can be channeled to the immune system.
Cheers–
MRE
I just love this blog. Just imagine the benefits of fasting 18-20h a day (which I’ve done for 3 months) – I’m eager to check out my inflammation markers and insulin levels.
This IF-lowers-cortisol-levels is very interesting. Caloric restriction (food deprivation) is known to increase cortisol levels.
Yep. I found the cortisol-lowering effect pretty interesting myself. I’m eager to see if it holds up in other studies.
MRE
As I have periodically mentioned. I have been intermittent fasting since April. Somone mentioned that their stomach disappeared. Mine did as well. Something else I experienced were lighter and shorter periods. My cycles once lasted 6-7 days and were heavy for a great portion of the cycle. Now they are around 5 days and lighter. I also have milder cramps and fibroid pain has dissipated.Also, I have a BM within a half hour after my first meal I can set my watch by my BMs. My fasting period is 20-22 hours. I eat one other meal following my “breakfast” and my gut feels so empty.
I am sure that the benefits of fasting isn’t eating less food as much as eating less often. Allowing a long amount of time for a fast gives the body time to complete the digestive process. This not only improves regularity but it also improves insulin sensitivity especially among low carbers. I always make sure that I eat nutritious low carb meals with a good amount of protein.I usually don’t even have an appetite for my second meal because of my insulin stability. I probably would skip supper if it weren’t for the fact that supper time is family time. We all sit down at the table as a family. Eating supper is a family affair. Since doing IF since April, I have lost 10 lbs. I notice that my body responds to exercise easily now. IF has made me very happy.
I’m sure that the advantages of the IF come from the eating less often. I’m glad you’ve done so well with it.
Cheers–
MRE
Dr. Mike, your comment to R. Francis Smith regarding speed-eating;-), I recall that in my teen and young adult years, I always ate slowly and family members would tease me.Not only did I eat slowly, I found it quite difficult to clean my plate.
Eating slowly – which I have great difficulty doing myself – is one of the best preventative tools against overeating.
Cheers–
MRE
Dr. Mike:
As you may know, many of us have been experimenting with IF since
your first and subsequent posts on the subject. First of all, thank
you for highlighting this area of research.
There are many of us on another forum who are interested in keeping
track of IF and medical related information for purposes of longterm
study. Many of us have followed IF for at least six months and more
are joining every day.
We would like to get your input on what data you think medical folks
might want us to capture and on what basis. Perhaps keeping this
data on ourselves would provide someone with good fodder for a study.
Here are the items we’ve thought of. None of us are
doctors/researchers and we really would value your thoughts on which
of these are good, which should be deleted, are there others that
should be added.
Here’s the list:Age
Sex
Weight
Goal Weight
Height
Bodyfat percentage as measured by what? Or BMI as calculated by
what? Or Waist to Hip ratio?
Blood Pressure
Glucose level
Number of days on IF
IF Pattern?number of hours per day, number of days per week, Type of
IF?water only then food, 0 cal beverages allowed, Coffee and cream
allowed, etc.
Nutrient info: Average calories, carbs, protein, fats?daily? Weekly?
Triglycerides
LDL/HDL and ratio
CRP
Homocysteine
Total Cholesterol
Electrolytes?
Weight loss on IF
Health effects of IF
I’d love for you to respond through your blog if possible since
others might want to take up these measurements as well.
Thanks so much for any time you could devote to this.
Appreciatively,
Kathy Baugher
Hi Kathy–
After giving this some thought, I would get the info you’ve mentioned above with the following additions or changes:
Body fat percentage as measured by a bioimpendance analyzer, which are dirt cheap now. Make sure you follow the manufacturer’s instructions explicitly to get accurate results. Or use the tables in Protein Power, which are just about as accurate as the bioimpedence analyzer, but a little more cumbersome to perform.
Getting a waist to hip ratio is good, then measure the change over time. Or even simply the change in waist circumference.
I would certainly get fasting blood glucose levels, but more importantly, get a HgbA1c, which is a measure of average sugar levels over time – a much more accurate measure of what’s really going on.
Fasting insulin level along with the fasting glucose.
Serum ferritin and changes over time.
A full blood panel including Alk ptase, SGOT and other liver enzymes to see changes in liver function with time.
A list of medications at the start and any change in medications along the way, i.e., on blood pressure meds, was able to get off after 2 weeks of IFing. That sort of thing.
What supplements, if any, are being taken. And if they’re taken during non-eating days.
Amount and type of exercise.
Smoking status.
Medical history, i.e., diabetes, heart disease, liver problems, etc.
If I were doing this in a clinic I would certainly want to know the food intake on a week by week basis, so I would have people keep a food diary.
I hope this helps.
Cheers–
MRE
I know about intermitting fasting and caloric restriction for almost 9 years… and i apply it since then…i strongly believe in it as i look far better then before, also people tend to think i am younger then i am… the way i came up with it was not by the studies but by research i did for muscle mass growth and wondered why always eating would not increase muscle tissue… then it became clear you body needed to be in a fasting state to increase it’s growth hormone again and then when eating this potential energy could become free (IGF-1 due to the IGFBP-1 due to insuline etc…blabla:))
but apart from that i apply IF by skipping breakfast (i am not hungry so why should i eat?) and try to hold on as long as possible (before i get really hungry) and then i eat a “healthy meal” (slow carbs, moderate fat, moderate protein). This is mostly about noon… (so when other people start to eat their second meal of the day). then i wait until 8-9pm before i eat again, mostly a larger meal…
I however do believe that the intermittend fasting priciple only needs to be applied on protein/fat nutrients and not on carbohydrates, some studies do confirm this (need to look it up again on pubmed). In nature you do not have to kill an animal to eat some carbs… just look for a tree and pick an apple or an orange! So i think you can eat carbs the whole day long but try to limit protein/fat meal to once or maximum twice a day…
What are you thoughts on this?
Best regards,
Yannick De Wit
My thoughts are just the opposite. I would say that based on my experience with a whole lot of patients that it is the carbohydrates that need to be restricted and the fat and protein that can be eaten throughout the day. If what you are doing is working well for you, my recommendation would be that you stick with it.
Cheers–
MRE
Thank you for starting a blog on this fascinating topic and to those who have contributed their comments. My introduction to intermittent fasting came as a result of viewing a presentation called ‘What is normal blood glucose’.
http://www.diabetes-symposium.org/index.php?menu=view&chart=33&id=322
The Power Point presentation shows the results of continuous BG monitoring of a number of subjects with what are considered healthy blood sugars eating what is considered a normal (carbohydrate-loaded) diet. Three key results of the study caused me to conclude that the blood glucose patterns, far from representing ‘normal blood glucose’, represent a normal response to an abnormal influx of glucose arising from carbohydrates.
1. There was a large BG spike after every meal containing carbs (all meals in
the study did).
2. The biggest BG spike came after a meal in the morning (around 8 AM).
3. BG virtually flat-lined in the night when no food was being consumed
and gluconeogenesis was producing glucose as needed to maintain BG levels.
http://www.diabetes-symposium.org/index.php?menu=view&chart=33&id=322
After being shocked into reality by this presentation I started to eat 2 meals a day. The first is at about 1 PM, the second at about 7 PM. I seldom snack. At least once a week I skip one meal and cycle for 24 hours or more without food. Initially I experienced some flu-like effects and periods of low energy. I attribute these to a detoxification process. Now my energy levels are way up. I have never felt better in as long as I can remember. But the most intriguing effect of IF from the perspective one who was a carbohydrate addict is the modest sense of hunger I feel even after extended periods without food. And when I do eat my appetite is easily satiated. I have also noted some very significant physiologic changes in my desire for fat (which of late has decreased) relative to my desire for protein. It is as if I seem to know what I need to eat and, more important, when I have eaten enough of it.
You said:
“The fast is probably going to do more good for the diabetic condition than all the supplements in the world. If I were going to list my top five supplements for type II diabetes they would be magnesium, lipoic acid, CoQ10, biotin, and carnitine. I hope those are a part of your list.”
These supplements are part of my list. However, instead of the racemic form of lipoic acid I use the R+form which is many times more effective. L-carnitive also seems to have some kind of synergism with lipoic aid. It is important to take about 500 – 750 mcg of biotin with every 100 mg of lipoic acid since lipoic acid depletes biotin. The timing of lipoic acid also seems to be important to maximizing its effect.
I am a type II diabetic (diagnosed in Feb 2005). I am currently on an IF, VLC, no-grain diet. For several months now I have been on IF. I record my body weight. % body fat and total body water every morning at the same time on a bioimpendance analyzer. I am just about to resume reading my fasting blood glucose. Since I have the Dawn ‘Phenomenon’ I normally take 2 readings an hour apart to see whether my BG is increasing or staying stable. After starting IF I began to see near normal FBG readings for first time. Other BG readings are well within limits for non-diabetics.
I look forward to future comments from you and others who subscribe to this blog. I like Kathy Baugher’s idea of monitoring key indicators while on IF.
I would also like to hear your thoughts at some point on insulin resistance which seems to be tied to an inability of glucagon levels to sense BG levels in controlling the synthesis of glucose.
Hi Dave–
Thanks for the link to the presentation. I haven’t watched all of it, but I will when I have the time later. What I have watched, though, pretty much accords with what I have seen in my years of clinical practice.
I think insulin resistance is a much more complex phenomenon than I thought it was just a few years ago. I’m busy reviewing the whole idea again in view of a lot of new evidence. When I think I have a more complete handle on it, I’ll post my thoughts.
Cheers–
MRE
Research I have found recently suggests that not only insulin resistance but diabetes in general is far more complex and individualized than was initially thought. Although the objective of this research project is to develop new pharmaceutical agents you may find the following article ‘New Insights and New Therapies for Insulin Resistance’ interesting.
http://academic.sun.ac.za/medphys/insulinresistance.htm
Hi Dave–
Thanks for the article. It’s been known for years that both insulin resistance and diabetes are much more complex than anyone thought at first. Here is a full text article that I think is one of the best I’ve read on the pathobiology of diabetes. Enjoy.
Best–
MRE
Dr Mike,
I’m very interested in what I’ve read in your various posts about IF, but I have a question.
While I’d like to try it, I’m wondering if, as someone who has had a gastric bypass, this method wouldn’t work for me, because I literally can’t eat all my calories in one meal, or one small window of say, three hours. For instance, this morning I had a protein shake when I woke up, then an hour later I couldn’t finish my breakfast of 1 egg scrambled with feta accompanied by bacon, and coffee with half and half. I guess I ate about 2/3rds of the egg/feta portion and maybe a couple strips of bacon (the bacon was served to me in a ‘wodge’ — that’s the technical term, heh, so I’m not sure how many strips there were). I probably won’t want anything more to eat for at least 4 hours after that. But while low-carbing (I’m doing a very-low-carb regimen, which is just easier and more pleasant for me right now) depresses my appetite, I do seem to empty out and get hungry every few hours.
Any thoughts on my situation?
Thanks!
You don’t have to consume all your calories in one meal. You can consume them in smaller meals throughout the time of the day dedicated to eating. Then you consume no calories during the portion of the day dedicated to fasting.
Cheers–
MRE
Help – can the fasting period be a different time of day?
I swim or run at 6 am on an empty stomach, and if I don’t eat afterward,
I get a terrible headache and lose all my mental power (get fogged).
Can my fast be from 2 pm to 8 am?
Also, it’s true that the male hunters would not eat all day while hunting,
but the women spend the whole day long gathering berries, roots, etc.,
and probably were constantly grazing until the men came home with the meat?
The fasting period can be whenever you want it to be. As far as I know there are no rules. The important thing is to let there be a lengthy time sometime during the day that the GI tract can rest.
What about in the winter? What did the women gather in the winter?
Cheers–
MRE
Dr. Mike;
Is it possible that a confounder in the CR studies was nutrient density versus calorie amounts? what I mean is that could the agent of benefit be not so much the calories, but the nutrient density of foods that has the most benefit? Gary Null mentioned this once long ago and I never heard it fully addressed anywhere.
Thanks!
BMC
Most studies of CR use food of the same nutrient density, but just less of them in the CR arm. So, although consuming foods with the greatest nutritional density is a good thing, I’m not sure it really figures in to the CR equation.
Well, I have to say that this is the first time I actcually read the entire study and I am amazed. I also would like to add that I have been IF since April 2007 and I honestly believe that my fibroid tumors are gone. Up until about 2 months ago, I cramped during and between periods. The exciting part is that I haven’t been cramping between periods but cramps are barely even noticeable during menses. My tummy even seems flatter and much less gassy. Also, I am working with people who all have the flu yet I remain disease free and guess who did not get the flu shot this year. I’m just sayin”…
Dr. Eades,
I was excited to stumble on your blog while researching fasting, as I am very impressed with Protein Power Lifeplan and use it as my nutrition and weight loss basic text.
I have lost 50 pounds and normalized my blood glucose with a low-carb 1500-calorie diet, but seem to be stalled at this point. I’d like to try the intermittent fasting. I would also like to follow the fast my church prescribes, which is no animal products from now until Christmas. I can’t eat soy or gluten, and nuts are too high in fat to get adequate protein without going over my calorie limit. Are there any vegan foods which can provide enough protein without excessive carbs or calories? What would be the likely result of two weeks of every-other-day fasting with limited protein?
Thank you.
Andrea
As far as I can tell, about all you can supplement with is rice protein powder. You would probably do okay on that from now until Christmas.
Great article: http://diabetes.diabetesjournals.org/cgi/content/full/54/6/1615?maxtoshow=&HITS=10&hits=10&RESULTFORMAT=&author1=brownlee&searchid=1&FIRSTINDEX=0&sortspec=relevance&resourcetype=HWCIT
Thanks!
This is a terrific article that came out four or five years ago. Well worth reading.
Is “fasting” while awake any different than not eating when you’re asleep? My family routinely at dinner at 5:30 pm and then that was it until breakfast, which was rarely before 7am,. We were not a snacking family. That would be 13 hours at a stretch, no hardship because you’re asleep for most of it anyway. These days my evening workout doesn’t even get me home for dinner until after 9pm, so even a small dinner means eating within an hour or two of bedtime, and only 9 or 10 hours.
It seems to me there must be some difference as I would have thought many, if not most, people have at least 12 hours between their last meal and their breakfast the next day.
Would one need to consume double the amount of protein your books suggest all in the one eating day? i.e. someone who needs to consume 100 grams of protein daily, would they need 200 grams daily with an alternating IF schedule?
Thanks for answering (if you get to it)
Hi Dr. Eades. I just jointed your blog and I am very much impressed at the amount of work and knowledge you put into answering ALL comments. It is unbelievable. I know what it means since I am also a webmaster. I see you also have a nice Alexa Ranking, 50.000. That is something you don´t get overnight.
Congratulations,
Alfredo E.
Hi Dr. Eades
This is an old blog so I am not sure it is still being followed, but let me query it anyway in hopes.
First I arrive here with a bit different mindset i.e. concerned with the inflammatory factors of food ingested and the ratios of Omega 3 fatty acids VS Omega 6 fatty acids. I reading much of the info on IF I am fascinated by the anti inflammatory response of the body and think it has real merit to be combined as part of the process of eating and living to a good health result. But I wonder about some of the discussion on present diet if the food choices had been determined by its inflammatory properties and how the total diet played out in the Omega 6 to Omega 3 ratios how it would have changed some of the decisions and then of course the results of the responses to food eaten. I personally have lost aobut 70 pounds since April 2009 just watching the inflammatory factors of foods and keeping my diet positive in an anti inflammatory way. I have also used the diet approach with fish oil for the mega omeaga 3 boost to dogs diets and am sucessfullly treating several inflammatorty based problems. I have taken two dogs off phenobarbitol for epilepsy and made remarkable improvment in another dogs severe cerebellar function to the point I have pulled his quality of life back up that I an no longer considering sending him over the bridge because of the constant trauma he was causing himself. I digress here too muchI think IF has a place here with both humans and our animals.
BTW there is some very good scientific data to document that type II diabetes is caused from the inflammatory status and not the fat itself (although fat produces inflammation into the body directly as well). Fat is an inflammatory disorder and should be looked upon as such. Until we do that the obesity epidemic will continue to exacerbate in every area and group. If IF deminished inflammation that in itself is a wonderful modality and with as much as a 20 residual, that is a true blessing that we should be able to harness and use with a proper diet that continues to stimulate anti inflammatory actions of our God given bodies. .
BTW I have driven down my hsCRP from 4.9 to just over 2 and my HDL/TG ratio is now 1.7 and I am still 275 pounds with a BMI of 39.7 (a lot better than where I began at 49.2 in April) I am using fish oil to help as well. Too much good news here to tell it all, I just want to share for the benefit of others.
Dr. Eades, Finally I read this blog and was quite blown away to learn how sinificant vitamins such as B12 and folic acid levels improve during fasting. As you know I have been practicing this for nearly 3 years. Now, I have come to the point in my low carb journey, where I need to come to a better understanding of what supplements I need to take and how I can improve low carb lifestyle. I have recently been diagnosed as pre-diabetic and anemic although I am quite healthy. The doctor wants me to adhere to my low carb lifestyle but I want to venture further into my journey to see how intermittent fasting affects my glucose.
Although I am anemic according to saturation and ferritin levels, I feel great. I understand the low B12 levels can affect my iron levels and was considering increasing my vitamin B12. However, I am questioning that decision now that I see that fasting can increase these levels naturally. Also, I have read that people who do various versions of IF have a natural tendency of higher glucose levels. That being the case, should highlight the importance of restricting sugar intake. I like intermittent fasting and plan on sticking with it for quite some time. I just want to share where I am at present with my journey.
Thanks Doc,
Mary
Hi, Dr. Eades,
I just found your wonder site via search engine & bookmarked it.
re. fresh meat & scurvy, as an “antarctic geek”, i have read quite a few books on early antarctic exploration/
when vitamin C was a hypothesis. for a while, some thought it was spoiled food that caused it. so Caption Scott’s team ate mostly canned food hence scurvy, perhaps Vitamin B deficiency as well in 3 months. & all perished.
While captain Shackelton believed in fresh meat (esp. organ meat). his team were on stranded on the ice for 18 months. they ate mostly a meat diet. no one got scurvy.
Amundson trained with Innuits so his team also ate fresh meat. also didn’t get scurvy.
i also heard that early Chinese ocean explorers in 15 century just carried beans & let
them sprout on board. so they didn’t get scurvy.
anyway, you may have known these.
regards,
I have been low-carb/paleo for a year now and am struggling with adrenal fatigue, hypothyroidism and estrogen dominance. I am a busy mama to nine, so my body has been through a lot. I have lost 50 pounds in the past year and feel I probably have another 15-20 to lose.
Is it possible/safe for me to do IF? I do have some pretty severe hypoglycemic reactions and hate being tied to food. I crash pretty bad if I don’t eat something every couple of hours. i would love to try this and am willing to push through the symptoms if I knew it was good/healthy for me. Is is possible to be too sick to do this? Any advice would be a blessing.
It’s probably okay for you to do IF. You may even feel better after a few days on the regimen. I’m not sure that what you have is adrenal fatigue. If you’re a mother to nine, it’s probably regular old fatigue that’s getting to you.
This is the first article that I read on fasting and inflammation. I have been suffering from severe pain and stiffness in my feet especially in the mornings and then pain all day. My knee has been swollen twice the size as the other for a year now. This last weekend my whole family got a stomach bug and I lost 8 lbs. I woke up around 4am and realized that my feet didn’t hurt… I got up and walked as if there was nothing wrong. My knee has decreased in the swelling by at least half. I did have a day that the pain came back during the day in my feet but then again this morning NO PAIN. Yesterday I ate only twice as I was feeling this stomach pain again. Realizing that it must be the fasting that is doing this. I slept better last night than I had in over a year. I’m going to do more reading on this and try and figure out how often to fast … but I feel like I have hope for the future in a less painful life. I am only 39 years old and I do have arthritis starting in both my feet, my left knee and my right middle finger. If you have any suggestions for me, I sure would appreciate any feed back. I am really excited about this. Finally hopeful!!!
First, you probably need to be checked out by a physician to see what’s causing your widespread arthritic pain at such an early age. Aside from that, you may want to add some krill oil and curcumin to your fasting regimen.
Thanks for your reply. I will try the krill oil and curcumin. I have talked with a physician and was tested for rheumatoid arthritis as it is in my family history along with other arthritis. I was only advised to take Aleve to help with pain and inflammation relief… that has only taken the edge off and I only take it on really bad days. I have always tried to avoid taking these medications and am really frustrated that at such a young age I’m taking it so often.
I don’t have a fasting regimen ….I don’t know where to begin as it was just this last weekend that I got the stomach bug and discovered this “natural” way of reducing the inflammation. I will be seeking a second opinion about the arthritis… but am looking for any suggestions on how often to fast and what to eat…and when so I can start a “regimen”. It was just this morning that I realized that the fasting and reduction in my pain and stiffness is related. My first thoughts on this was that I was maybe having a food reaction and after being sick had cleared my system of it. Then this morning was more convinced it was the fasting since I did eat yesterday but was only limited to a couple times. Now I need to read up and figure out where to find help. Any advice on how to start is certainly welcome.
I would start by reading this post of mine on intermittent fasting that’s a few years old. It will give you some basic info to get you started. But I would still get worked up or, at the very least, question the physician that checked you for rheumatoid arthritis and find out what he/she found out.
THANK YOU!!!! I will check this out and speak more with my doc and still get a second opinion.
I appreciate you taking the time to respond to my questions and concerns.
Hi Dr.Eades. I was wondering how many calories and/or what blood sugar level stimulates an insulin response. I was wondering that to know the maximum number of calories of carbs you can eat while still giving your body a complete rest from insulin (ie is it 25, 50,100). I realize it is probably different for different people but on average what is it ?
Also I am planning to do intermittent fasting and drink green tea, coffee, and/or cocoa (all in water without sugar) on the fasting days. Is that okay ? Is caffeine okay while fasting ? Is it synergistic, counterproductive, or neutral ?
Also what is the maximum amount of calories that would be considered negligible on fasting days ?
I did try to google for the answers first but could not find anything. Thanks for the opportunity to ask you questions. Looking forward to your reply.
I spent several years IFing to a certain extent. During the week, I’d have my only meal at 4 pm. I had NO hypoglycemia feelings or weakness, but I would fall asleep soon after eating. In time, I developed palpitations and controlled them through Inderal.
3 months ago, I was diagnosed with hypothyroid (who knew that Inderal suppressed T3?) and adrenal exhaustion. Looking back, I believe these problems were caused by IFing and further exacerbated by the Inderal. So, now I’m starting to eat breakfast and to keep up my meals. As easy as IFing was, I wont’ do it again.
I have been fasting everyday for 20 hours each day for 2 months. My goal was to do this during the week, but so far, I have done it 6 days per week. It is not the most socially friendly eating schedule. My work shift, noon – 9pm really makes it possible. I eat from 8pm to midnight.
I’m not getting a doctor’s supervision, but I am going to go get some blood work tomorrow. I have had a publicly offered cholesterol test a year ago and my total cholesterol was 136. Yesterday I had another one and it was at 190. Blood glucose was 90 after fasting for 14 hours aside from a teaspoon of honey with my coffee 6 hours earlier.
I want to verify if 190 was accurate and discuss this diet with my GP. Let me know if you would like me to follow up with the results. I am very interested to know if this diet could possibly contribute to a higher cholesterol level and why. This time I will get a full breakdown of all the cholesterol levels with a true 12 hour fast.
I have experienced absolutely no ill effects as a result of this diet. I make sure I am eating fruit and veggies during my window, but find that I am craving something heavy along with it. Also, sweets are welcomed. I have been working out all during this time. 30 min cardio 4 times a week and weights 4 days a week. I find I have an abundance of energy.
Having read several books on fasting,and becoming very interested,I tried the lemon cleanse fast. It was the second time I had fasted,the first time was four days.The last time was thirteen days.the incredible thing I found was after the initial four days my energy level was high and remained so steadily for the entire fast! Yes I lost some weight,started at 265 and was 238 on thirteenth day.My intention in fasting was for internal house cleaning. I felt great for the duration of the fast.I do want to say I told no one of the fast because I knew they would try to sabbatage my efforts.You have to be mentally prepared to do it and absolutely be confident with the end results.the lay person will attempt to scare you to death! Oh my god!,you missed how many meals? Anyway just wanted to share that with you all Happy Fasting!
Interesting notes on the inflammation markers post-Ramadan and tying it into intermittent fasting.
Then there is the documented case from the 1960s of the 27 year-old Scotsman who fasted for over a year (under close medical supervision). He lost 276 pounds and was fine. He didn’t gain the weight back.
I do IF daily. In other words, I generally have my first meal of the day after 3:00 in the afternoon. THe later I can go before eating my first meal, the better, although I do not force it. I make a concious effort to eat healthily and I eat nutrient dense food to manage my health. My diet is low carb/almost paleo. I eat a vast array of meats, vegetables. Even my treats are healthy such coconut cookies and macaroons. I began making my homemade bone broths and include coconut oil and butter in my diet. Homemade mayo is next on my list. Hy health has improved over the years that I have been low carbing and fasting…no brain damage yet.